Epileptologists at the CHOC Neuroscience Institute and UC Irvine biomedical engineers have devised a novel approach to pinpoint precise targets for surgical resection or ablation as a means to control epileptic seizures in children. The approach uses densely spaced electrodes to map high-frequency oscillations (HFOs), which tend to be most prevalent in seizure-producing brain tissue. This research offers new hope for the approximately 50% of patients who still experience seizures after surgical intervention. It also has the potential to prevent unnecessary surgery.
HFOs recorded from electrodes inside the brain or on its surface help pediatric epilepsy specialists and neurosurgeons determine which brain regions should be removed or ablated during epilepsy surgery. Historically, most HFO research has not accounted for electrode size or the distance between electrodes when analyzing the use of HFOs to identify diseased brain tissue, believing these recording characteristics to be irrelevant. This new approach challenges that notion and seeks to improve identification of seizure-generating tissue through multi-scale recordings. Additionally, mapping brain function with this high-density electrode array allows more targeted surgeries, enabling resection or ablation with less post-operative morbidity and functional deficits.
The research is being conducted courtesy of a $1.8 million grant from the NIH National Institute of Neurological Disorders and Stroke. Awarded to UC Irvine’s Dr. Beth Lopour, the five-year R01 grant aims to develop and validate computerized tools that would improve identification of the seizure onset zone. Pediatric epileptologists and neurosurgeons at the CHOC Neuroscience Institute are collaborating with UCI biomedical engineers on the research.
Recording signals from the brain
HFOs hold the key to CHOC’s ongoing research. When a pediatric patient does not respond to seizure medication, electrodes are often implanted into the brain or onto its surface to monitor abnormal electrical activity and capture seizures. The neurologist then uses the collected data to determine surgical candidacy.
Standard intracranial grid electrodes are spaced 10 millimeters apart, from center to center. In this study, on the other hand, researchers utilize a high-density grid with electrodes spaced only 3 millimeters apart. They hypothesize that closer electrodes will lead to a greater amount of diagnostic information and an enhanced ability to pinpoint the source of seizures.
With this enhanced capability, neurologists have already seen preliminary success. Early data was submitted as part of the NIH grant application, according to Dr. Joffre Olaya, pediatric neurosurgeon at CHOC, and one patient recently received a successful resection. The team hopes to enroll 35 patients with pediatric epilepsy in the study.
Reducing deficits and avoiding unnecessary surgery
“We review a lot of data before concluding someone is a surgical candidate,” Dr. Olaya says. “Based on pre-op workup, we focus our evaluation on a certain area of the brain to narrow down the source of seizures. We hope this study will help us narrow our focus even more, so we can diagnose troubling areas with greater precision.”

When the area of surgical focus is housed within structures in the brain that govern critical functions, providers must consider the risks and benefits of surgery over any potential deficit. Being able to precisely locate a troublesome area helps physicians determine and reduce potential risks with greater exactitude. As a result, physicians and patients are better prepared to make educated treatment decisions.
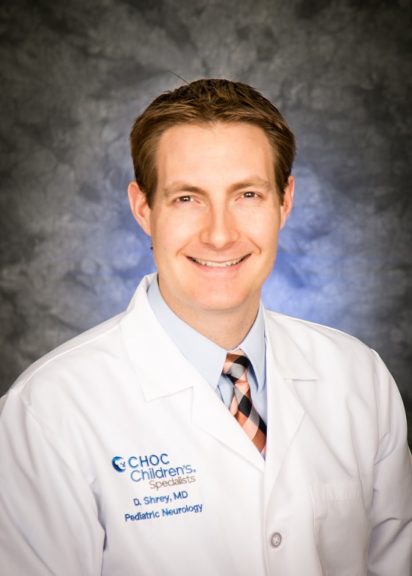
“We believe that our novel techniques will help to identify patients who would not significantly benefit from surgical removal of brain tissue and therefore allow them to avoid unnecessary and ultimately unsuccessful operations,” says Dr. Daniel Shrey, pediatric neurologist and epileptologist at CHOC. “In instances where no seizures or an insufficient number of seizures are captured during intracranial monitoring to make a clinical decision about surgery, we hope that including HFO data will give us sufficient confidence to pursue surgery, when appropriate.”
Expanding the scope of epilepsy knowledge
By collecting novel data from patients with epilepsy, CHOC pediatric neurologists are adding to the collective knowledge of the disorder. Their hope is that the medical world will gain new tools for diagnosing and treating one of the most common childhood neurologic disorders.
“We’re fortunate to have such a wonderful collaboration with UC Irvine,” Dr. Olaya says. “This is truly a team effort, and it’s exciting to have the opportunity to do this important project together — one that increases our ability to provide patients with freedom from their seizures.”

CHOC Hospital was named one of the nation’s best children’s hospitals by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings and ranked in the neurology/neurosurgery specialty.