Pathways After Cancer Treatment (PACT), a new bridge clinic at CHOC, helps support the mental health of teen and young adult cancer patients.
Determining the role of regulatory T cells in successful immunotherapy
CHOC researchers seek to study the role of Tregs in whether pediatric leukemia patients treated with CAR T-cell therapy experience a relapse.
Young leukemia patient is part of several oncology research studies
Max, CHOC patient with acute lymphoblastic leukemia (ALL), participates in cancer research trials to improve outcomes and treatments.
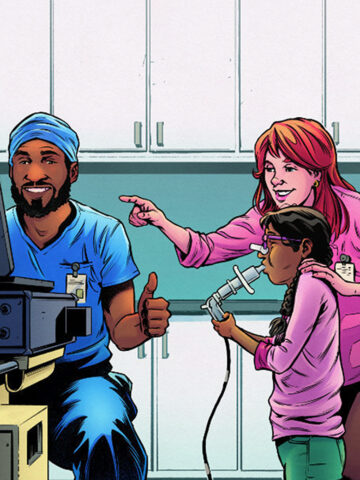
Kazaam! Comic Assent earns kudos as tool for young patients to better grasp research studies
Colorful comics aid young patients in understanding and providing assent for participation in research studies to advance treatments.
Working to improve leukemia outcomes with advanced research
Physicians at CHOC lead a new study to improve survival rates of children with pediatric acute lymphoblastic leukemia (ALL).
Leukemia stopped her in her tracks, but not her willingness to participate in oncology studies
A CHOC AYA oncology patient uses her experience to give back to others by participating in ongoing cancer research and clinical trials.