CHOC, in partnership with UC Irvine & Chapman University, received a grant to screen patients for adverse childhood experiences.
CHOC telehealth visits continue at a rapid pace
Virtual visits with a CHOC provider via a smart phone, tablet or computer are here to stay and expected to continue growing at a rapid pace.
Dr. Mary Zupanc awarded prestigious Arnold P. Gold Humanism in Medicine Award
Dr. Mary Zupanc has achieved many awards, but considers the Arnold P. Gold Foundation Humanism in Medicine Award her highest honor of all.
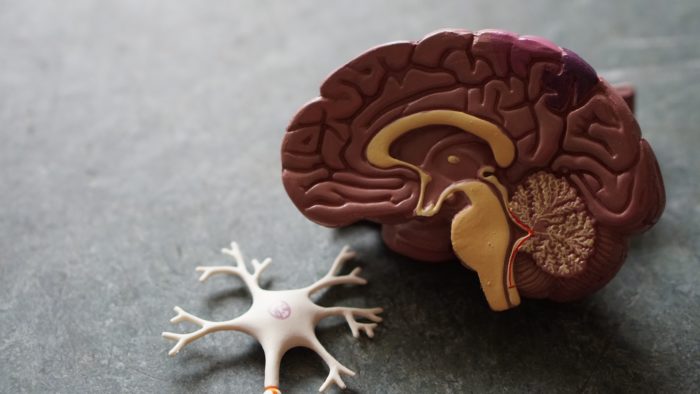
The transition from child to adult care must start early with education, pediatric neurologist emphasizes
Dr. Mary L. Zupanc discusses why she’s passionate about preventing patients transitioning to adult care from falling through the cracks.
Investigational Drug Study Leads to FDA Approval for Fenfluramine in Treatment for Dravet Syndrome
Dr. Mary Zupanc was a key investigator in a study that led to FDA approval for a medication to treat children with Dravet syndrome.
5 things pediatricians should know about seizures
Dr. Mary Zupanc points to five important points pediatricians should consider when seeing a patient who has had one or more seizures.