The event drew participants from representatives of eight children’s hospitals, 15 organizations, and a total of 200 attendees representing 20 states and four countries.
Rare mitochondrial diseases are the focus of Feb. 10 virtual CureARS event
The upcoming webinar is open to the public, and will share the latest developments in the battle against rare mtARS mitochondrial diseases.
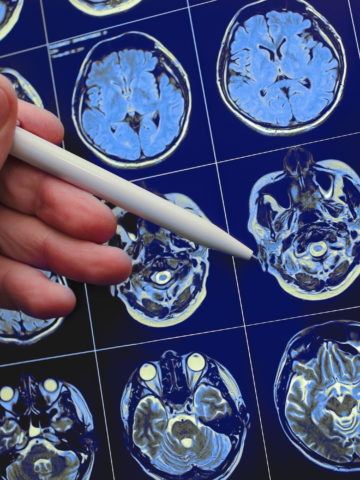
CHOC leads 21-center study to find predictive biomarkers for infantile spasms, a rare and dangerous type of epileptic seizure
In a 21-center study, CHOC hopes to discover early treatment strategies for infantile spasms, a rare and dangerous type of epileptic seizure.
Rapid Whole Genome Sequencing continues to provide answers and hope for parents of critically ill children with rare diseases
CHOC has ordered cutting-edge tests of rapid whole-genome sequencing (rWGS) on 150 patients, with 76 of them getting a precise diagnosis.
Rapid genome testing for infants saves lives, costs
A recently completed pilot program at CHOC and other California clinical sites helped target a baby’s specific genetic disease in just days.
Journey to a rare diagnosis: Colten’s story
A CHOC PICU nurse tells the story of her son, Colten, who received a rare Alström Syndrome diagnosis with the help of specialists at CHOC.